Mark Brezinski MD, PhD
(RESEARCH BIOGRAPHY AS OF 2023 OCT and Non-OCT)
Mark Brezinski MD, PhD
(RESEARCH BIOGRAPHY AS OF 2023 OCT and Non-OCT)
BRIEF RESEARCH BIOGRAPHY
General
Mark Brezinski MD,PhD (H index =58) is best known for achieving Optical Coherence Tomography (OCT) imaging in nontransparent tissue (including coronary arteries), when previous groups had failed, but his research achievements extend OCT. He has spent most of his career at Harvard, MIT, Massachusetts Hospital, and Brigham and Women’s Hospital (greater than 25 years). He is a basic scientist, engineer, physician, quantum physicist, and medical educator. He not only trained with Allen Lefer PhD (Thomas Jefferson University) and Charles Serhan PhD (Harvard Medical School), but Nobel Laureates including Bengt Samuelsson PhD and E.J. Corey PhD. He did cardiology fellowship at Massachusetts General Hospital (MGH), where he would ultimately become an attending first at MGH then BWH. He has had approximately 15 NIH RO1s, at times having five at one time. He has published approximately 150 papers. He is the winner of numerous awards including the Presidential Award for Scientists and Engineers, Young Investigator Award from the America Heart Association, and Top 20 Investiagtors in the 100 Year History of Brigham and Women’s Hospital (BWH) . Dr. Brezinski’s pioneering work can be confirmed from many sources, including in PNAS (https://doi.org/10.1073/pnas.231388312) for the 2023 Lasker Award “Cardiology is currently the second-largest clinical application. Intravascular OCT was pioneered by Mark Brezinski. He approached our group and proposed this area of research. Brezinski led the first studies demonstrating that OCT could detect vulnerable plaques, which cause sudden cardiac arrest. He also led OCT studies in many different areas: imaging gastrointestinal, pulmonary, and urinary tissues, different cancers, nervous tissues, surgical guidance, and fiber optic catheters for internal body imaging.”
Pre-OCT Work: He began doing formal research in 1984, with a focus on studying thromboxane inhibition in the treatment of myocardial infarction (MI). Thromboxane receptor antagonists are being examined to replace aspirin in preventing MIs, as they are more specific. He also has a strong background in quantum mechanics then fiber optic engineering. In addition, he did some of the earliest work on lipoxins. In 1990, prior to his OCT work, he identified a downregulation mechanism of inflammatory cells (membrane incorporation of 15-HETE) published in PNAS. Analogies for 15-HETE are being evaluated as anti-inflammatories, including the treatment of COVID.
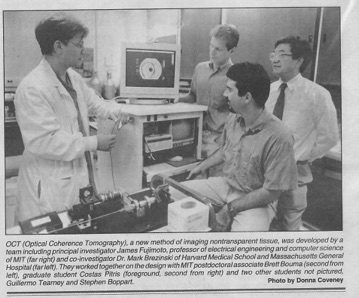
With these advances, the first demonstration of endoscopic OCT was reported in 1997 in the respiratory and gastrointestinal systems of a rabbit. The first demonstration of intravascular imaging was done in 1999, where blood had to be flushed out of the field (https://doi.org/10.1136/hrt.82.2.128). Dr. Brezinski directly compared OCT with IVUS, demonstrating the superiority of the former (https://doi.org/10.1136/hrt.77.5.397
). The first TD-OCT imaging catheter and system was commercialized by LightLab Imaging, Inc., formed in 1997 by Prof. Fujimoto, Mr. Swanson, and Dr. Brezinski. In 2001, Dr. Brezinski developed index matching to allow imaging through blood (https://doi.org/10.1161/01.CIR.103.15.1999). Intracoronary imaging in humans was achieve in 2003 by the Tearney and Bouma group (doi:10.1136/heart.89.3.317). Dr. Brezinski and Professor Fujimoto could not pursue in vivo human imaging because of COI. OCT systems began selling significantly in 2007. Lightlab Imaging is now owned by Abbott labs who has run double blind prospective trials showing morbidity and mortality benefits (DOI: 10.1056/NEJMoa2307770). "Among patients with complex coronary-artery bifurcation lesions, OCT-guided PCI was associated with a lower incidence of MACE at 2 years than angiography-guided PCI." A list of studies can be found on the Abbott web site. The only significant differences between the original LightLab system and those used in the clinical trials, besides using SS-OCT, is a rapid catheter attachment system to the OCT engine. Many advances which have been developed since 2000 which have not been incorporate in vivo by clinicians or in clinical trials. This includes PS-OCT, OCT elastography, and an OCT guidewire. Since 1993, he has advanced OCT through basic science, engineering, clinical trials, quantum physics, and classical physics. His major areas of OCT research are cardiology, osteoarthritis, quantum field theory of OCT, and adjuvant OCT techniques (PS-OCT, elastography, second order correlation spectroscopy).
Other Fields
Prior to 2000, Dr. Brezinski (with James Fujimoto PhD) would be the first to demonstrate OCT imaging for osteoarthritis (OA, discussed below), cervical cancer, esophageal cancer, bladder cancer, microsurgical guidance, breast cancer, prostate cancer, nerve repair, and tissue engineering.
OCT in the Diagnosis of Pre-Osteoarthritis (Pre-OA)
Dr. Brezinski has also done extensive work with OCT in diagnosing pre-OA, OA at reversible stages, in collaboration with orthopedic surgeon Scott Martin MD. This work spans more than 25 years. Initial work in the 1990s showed that OCT could diagnose early OA, but PS-OCT could diagnose pre-OA (PMID: 10090174)(PMID: 1140912). Pre-OA here is cartilage normal by visualization or MRI, believed to be at reversible stages. PS-OCT is identifying collagen disorganization. The first in vivo study was in patients undergoing knee replacement (https://doi.org/10.1186/ar1491). Dr. Brezinski would continue this work in the new millennium with most recently a double blind clinical trial in 2022 (https://doi.org/10.1016/j.ocarto.2022.100313). In this trial in patients undergoing arthroscopic meniscal surgery, abnormal PS-OCT predicted the onset of OA in 2.8 years.
OCT Work (2000-present)
General
After 2000, building his own OCT systems at Brigham and Women’s Hospital, he would go on to produce many of the most important OCT papers for the next 20 years, including inventing quantum second order correlation spectroscopy. Again, because of his IP (and owning LightLab), he could not participate in cardiac clinical trials because of COI. His collaboration with James Fujimoto PhD would be sporadic as they moved into different areas. He was continuously funded for more than 20 years, at times having five simultaneous NIH RO1s. He is the author of the Textbook of OCT where he wrote all chapters (physics, engineering, and clinical applications) except the clinical trials chapter (ISBN: 9780121335700).
PS-OCT
Polarization sensitive OCT (PS-OCT) differentiates organized regions of collagen from disorganized. Dr. Brezinski began working with single channel PS-OCT prior to 2000 with manuscripts on cartilage, diagnosing pre-OA. Dr. Brezinski’s group is the only group that uses single channel PS-OCT, which measures relative rather than quantitative PS-OCT like dual channel. His group compared both approaches and found single channel was less susceptible to artifact (ttps://doi.org/10.2147/RMI.S4389). Dr. Brezinski has used single channel PS-OCT in multiple in vivo human intraarticular joint studies described above. In 2006, Dr. Brezinski demonstrated PS-OCT could differentiate, in coronary arteries with atherosclerosis, organized from disorganized collagen (DOI:https://doi.org/10.1016/j.ijcard.2005.11.036)
Elastography
OCT elastography measures the mechanical properties of tissue without tissue contact. OCT images are performed with and without applied pressure. The differences in the OCT image at the two pressures, after image processing, yields the elastic modulus. The pressure can be applied with many approaches including ultrasound or blood pressure variations. Three papers by Dr. Brezinski are particularly notable. He published the first demonstration of OCT elastography in arteries (https://doi.org/10.1136/hrt.2003.016956). The second paper refined the technique by establishing the elastic modulus with tissue phantoms as well as arteries (doi:10.1259/bjr/22522280). Different weights were applied and the amount of compression measured with calipers and OCT. Once the modulus was defined for phantoms and arteries, OCT elastography was performed to calibrate the technique. The third paper demonstrated when changing applied pressures, the tissue needs to reach steady state (the tissue response is not immediate) so pulsed techniques are unlikely to be accurate (doi:10.4172/2469-410X.1000112)
. In addition, this paper calculates the pressure of IVUS ultrasound far exceeds the elastic modulus of the tissue, estimating IVUS elastography is not a viable technique.
Ultrasound Modulated OCT
In the first article in PNAS, Dr. Brezinski demonstrated the use of a parallel ultrasound beam with OCT(https://doi.org/10.1073/pnas.1421558). This improves penetration and image quality. The theoretical basis is discussed in the paper. The second paper is in the Journal of the Optical Society of America (https://doi.org/10.1364/JOSAA.25.000938). This is a quantitative paper looking at different ultrasound frequencies and amplitudes. The work showed photon - phonon interaction behaves similar to the photoelectric effect rather than the classical linear responses expected.
Quantum Field Theory of OCT
Dr. Brezinski published “A Quantum Field Approach for Advancing Optical Coherence Tomography Part I: First Order Correlations, Single Photon Interference, and Quantum Noise” (doi: 10.4172/2469-410X.1000176). This is the only work examining the quantum physics of OCT. Parallels exist with work on detection of gravitational waves. OCT operates by first order correlations from a quantum mechanics viewpoint, where single photons interfere with themselves along indistinguishable paths (more accurately the paths interfere).
Technology Advances
In addition to the technology advances already described, Dr. Brezinski would advance SS-OCT technology(https://doi.org/10.1364/AO.47.006151). He demonstrated that SS-OCT had worse dynamic range than TD-OCT. He would then move on to partially improving this true logarithmic amplification (https://doi.org/10.1364/BOE.2.001769), which is patented.
SOC spectroscopy will be discussed below as it is not OCT, but can be used simultaneously with OCT.
Other Areas of Dr. Brezinski’s Research
Acute Coronary Syndromes (ACS) Pathophysiology
Dr. Brezinski has studied ACS and coronary plaque pathophysiology since 1984. Three papers written in this millennium will be emphasized here. The first involved an OCT case study and then analysis of prior histopathology (doi: 10.1016/j.ijcard.2014.09.144). The patient had PCI for ACS where an acute coronary occlusion occurred just after stent placement, but millimeters distal to the stent and original culprit lesion. There were two ruptured TCFAs in the imaging, the culprit lesion and one distal without a clot. The target lesion was associated with a long necrotic core while the other TCFA was not. The long core was evacuated on stent placement (which penetrated the intima), leading to the distal clot. Till this time the Brezinski group and other groups focused on plaque in cross section. The conclusion of the paper was that TCFAs associated with long necrotic cores were more prone too ACS. Subsequently, Dr. Brezinski’s group and groups analyzing OCT registries began including measures of core length. As long core evacuation is uncommon, the mechanism why long cores are associated with ACS remained unclear. In a paper in early 2019, Dr. Brezinski proposed long cores lead to failed healing after plaque rupture or erosion (doi:10.1001/jamacardio.2019.0312). Related to the second paper, for 30 years, based originally on a 1980s NEJM paper, it was believed plaque angiogenesis destabilized coronary plaque and increased the risk of MI. So in a second paper published in Circulation (December 2019), analyzing coronary histopathology and the data from the original NEJM paper, Dr. Brezinski proposed angiogenesis was critical in stabilizing and not destabilizing plaque (DOI: 10.1161/CIRCULATIONAHA.119.042192). This was supported by data from patients receiving angiogenesis inhibitors who have an increased, and not decreased, risk of coronary thrombosis. When a plaque ruptures, it takes days to more than a week for a clot to be occlusive. If the vessel wall contains specialized smooth muscle cells and endothelium, they enter the clot and stabilize it preventing MI. If the region lacks angiogenesis, which comes from the adventitia and can not penetrate necrotic cores, there is no cellularity to stabilize the clot. The proposed mechanism of plaques which lead to ACS is that they have a long necrotic core (or similar obstruction) which prevents angiogenesis from reaching areas of the intimal surface. Cellularity is lost and on plaque rupture (erosion) the thrombus grows to the point of occlusion.
Quantum Thermal Second Order Correlation Spectroscopy
Thermal second order correlations (SOC), thermal source produced photon pairs interfering with themselves along indistinguishable paths, has been treated classically till recently. These are removed in OCT systems via dual balanced detections as they are viewed as a noise source. In an article in Physical Review A, Dr. Brezinski demonstrated that these SOC have quantum mechanical properties and can be used to characterize tissue, specially lipid versus water-based tissue (doi: 10.1103/PhysRevA.78.063824). A patent has been issued of a more practical design, but experimental results from this system have been presented but not published.
COVID YEARS
Between 2000 and 2003, Dr. Brezinski’s research efforts were greatly reduced as he worked full time taking care of inpatient COVID patients.